Definition
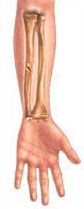
A fracture is a break in a bone. The physical force producing the fracture can also injure the surrounding muscles, ligaments, and other soft tissue.
Normally bones are strong and hard, but they are also somewhat elastic, particularly in children. Bones in young children bend much like the soft branch of a beech tree, developing cracks without actually breaking (green-stick fracture). The bones in older adults tend to be more brittle so that when bent or twisted, they break either crosswise or at an angle.
Types of Fractures
 |
 |
 |
 |
| Oblique Fracture | Comminuted Fracture | Spiral Fracture | Compound Fracture |
 |
 |
 |
| Greenstick Fracture | Transverse Fracture | Simple Fracture |
Diagnosing a Fracture
Broken bones may occur just about anywhere and anytime – on the ski slopes, during an automobile accident, or in the home. The usual symptoms include:
- Localized pain made worse by movement
- Inability to use the affected area
- Tenderness and swelling
- Deformity of the area around the fracture
- Muscle spasm with slight movement
- Feeling the bone ends grate together
An x-ray of the involved bone(s) is usually needed to confirm the diagnosis. Outward appearances are deceptive; some apparent fractures are not breaks.
Infrequently, even x-rays are not conclusive. Mistakes most commonly occur in the diagnosis of stress fractures. If a fracture is suspected but not seen on x-ray, repeat films, done 10 to 14 days later, or special studies such as a bone scan or a MRI may be needed to identify the fracture.
Treatment of Fractures
After a fracture has been diagnosed, treatment begins by realigning, or “reducing,” the affected bones.
Closed Reduction – Without cutting open the fracture site, an orthopedist uses the sense of touch to feel the fracture beneath the skin and, with the help of three-dimensional x-rays, realigns the bone. Once the bone is back in position, a plaster cast immobilizes the area.
Open Reduction – A doctor surgically exposes the fracture site, manipulates and realigns the exposed bones, and inserts an internal metallic device, such as a plate or pin, to maintain rigidity. Hip fractures may require replacement with a prosthesis. During surgery, the operating doctor carefully protects undamaged tissue in the area and preserves the blood supply to the fractured bone fragments.
Some fractures in which bones are not severely displaced are treated by external splinting without bone manipulation. Other fractures may require only a protective device such as an arm sling. Open fractures require specialized emergency treatment to minimize the risk of infection.
Once bones are realigned, they must be immobilized until healed. Healing takes place when the tissues produce a substance called callus that binds the bony fragments together. Plaster of paris casts may be used to immobilize smaller fractures in extremities, such as a broken arm, whereas traction may be necessary to immobilize larger areas, such as a fractured thigh bone.
The time required to heal a fracture varies with age, the location, type of fracture, and the blood supply to the area. Fractures heal more rapidly in children – a fracture that take 3 weeks to heal in a 4-year-old would take up to 3 months to fully mend in her mother. A long and slanting fracture knits faster than one that runs directly across the bone because of the larger surface area available for healing.
Immobilization of a joint carries risks. The surrounding muscles may atrophy and cause stiffness. A physical therapist can recommend exercises to keep the muscles and joints in good condition to help speed recovery.
Rehabilitation Therapy
While immobilization is the only method for encouraging fractures to mend, paradoxically, movement is also an essential component of the final healing process. After casts and pins are removed, the muscles of the affected area are stiff and atrophied. Graduated exercises improve both strength and flexibility, allowing you to regain full use of the area. Exercises, however, should be approached cautiously or you will suffer injuries to unconditioned muscles and ligaments.
Additional Support
Law Offices of William “Wild Bill” Weiss
130 Sutter Street, 7th Floor
San Francisco, CA 94104
Toll Free: 1-888-MC-CRASH (1-888-622-7274)
Local Phone: (415) 362-6765
Fax: (415) 362-2405
Office Hours: 8:30am-5:30pm, Pacific Time, Monday-Friday
E-mail: wildbill@wildbill-law.com
OTHER RESOURCES
MedlinePlus
New Ways to Heal Broken Bones
Fracture Index
Other Bone Disorders
Joint Related Problems